
Common Treatable Vein Conditions
Learn symptoms of:

What Are Spider Veins?
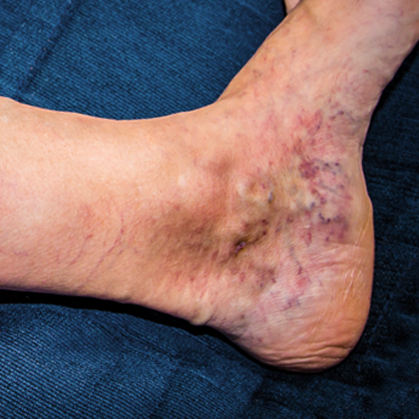
Spider Veins (Telangiectasia) are tiny red, blue or purple blood vessels that generally appear on the face, neck and legs, but can develop anywhere on your body. Visually they appear as a cluster of vessels (resembling a spider’s web) and are common in people over 50, but may appear as early as your 20s. Although they can develop in males, they frequently appear more in females. Spider veins are generally harmless, but in some cases they can cause discomfort, throbbing, aching, swelling, or even a burning sensation and tend to worsen throughout the day, especially if you have been on your feet.
Causes of Spider Veins
Aside from their appearance as clusters of red veins, spider veins may cause uncomfortable symptoms including a heaviness and dull aching in your legs, swelling, warm to the touch and tender, sores and rashes, throbbing, cramping, restless legs, discoloration, and itching around the veins.
Symptoms of Spider Veins
While venous insufficiency (weakened or damaged valves) is the leading cause of spider veins, other factors may predispose an individual to develop this condition: sitting or standing for extended periods of time, weight gain, hormonal fluctuations, heredity, taking birth control pills, history of blood clots, aging, constipation, and sun exposure. You can lower your risk of developing spider veins by wearing compression socks, wear sunscreen, eat healthy and maintain a healthy weight, along with exercising regularly.

What Are Varicose Veins?
Varicose veins are enlarged, swollen veins visible above the surface of the skin. They often appear bulging and twisted, dark purple or blue in color, and are most commonly found on legs or feet, where blood vessels work hard to pump blood back towards your heart, although they can occur anywhere in your body. Healthy veins in legs contain one-way valves, directing blood flow upward towards your heart. When valves become diseased and don’t close properly or fail to function, blood flows in the opposite direction causing veins to swell (up to four times their normal size). The increased pressure can be painful and cause a burning sensation.
Some varicose veins cause no pain, although it is less common, but may be a visible warning sign of other circulatory conditions. They can range in size and severity sometimes taking years for visible signs to appear, but they generally don’t recover on their own. Often they can be seen in people with occupations that require extended periods of time sitting, or standing, but also can occur during pregnancy. Hemorrhoids are also a form of varicose veins. Varicose veins can occur in either sex, but they are more prevalent in women.
Signs and Symptoms of Varicose Veins
Varicose veins are diagnosed with a physical exam and ultrasound to check blood flow, along with reviewing symptoms you’re experiencing. Although some varicose veins may not cause pain, highly visible signs include protruding and twisting veins that appear dark purple or blue on the skin’s surface. When varicose veins do turn painful, signs and symptoms include: a heavy, tired feeling in your legs, painful inflammation, swelling around your ankles, discoloration, itchy veins, a burning feeling and in severe cases you may develop ulcers or blood clots. Standing or sitting for a prolonged period of time can increase pain.
Risk Factors and Complications for Varicose Veins
The risk of developing varicose veins increases with the following factors: family history, gender (females are more inclined to develop varicose veins), hormonal changes during pregnancy, age (50 and above), obesity and occupation (jobs that involve prolonged periods of time, standing or sitting). And although uncommon, complications of varicose veins can develop: highly painful ulcers may emerge on skin near varicose veins, notably near the ankles, Thrombophlebitis (an inflammatory process) causes blood clots to form and block your veins, and bleeding (although slight) may occur with veins that rupture close to the skin.
What Are Venous Insufficiency Wounds?
Venous insufficiency occurs when valves in leg veins fail and aren’t effectively returning blood back towards the heart. Because the valves are damaged, blood flows in both directions, causing blood to collect within your leg veins. If not addressed, venous insufficiency creates pressure on the surrounding tissue and skin, leading to pain and swelling. Skin can turn a brown color called brauny edema making it look like you’re wearing a brown sock. If left untreated for a prolonged period of time the back pressure on your veins will prevent the inflow of newly oxygenated blood to the tissue, allowing tissue at the most vulnerable areas to die off. The result is a visible open sore called venous stasis ulcer, and can become infected if not treated.
Symptoms of Venous Insufficiency Wounds
Early signs of venous stasis include itching, discoloration, and tingling, along with your skin looking dry and thin. If not treated your skin may harden and turn a dark red, purple and brown color. You may also experience swelling, cramping and heaviness in your legs, especially when standing. As your skin breaks down an open wound or ulcer forms and fluid may seep out.
Causes and Risk Factors of Venous Insufficiency Wounds
Leading causes of venous insufficiency include Phlebitis, a history of Deep Vein Thrombosis (deep vein blood clot), smoking, cancer, and high blood pressure (in the leg veins). It’s also more commonly seen in females, older adults, pregnant, over weight, tall, family history of this condition, inactivity, muscle weakness, and standing or sitting for prolonged periods of time.
